History
Breast mass
The following may be seen in those with a breast mass:
-
Palpable mass (typically unilateral)
-
Family history of breast disease (malignant or benign)
-
Early menarche (< 12 years) and obstetrical parity (nulliparity)
-
Late menopause (age >55 years)
-
Associated symptoms of pain, nipple discharge, and skin changes (eg, dimpling or inflammation, nipple inversion)
-
Length of time present, speed of growth
-
Nipple itchiness without lump (Paget disease) [13]
Mastitis
The following may be seen in those with mastitis:
-
Localized breast erythema, warmth, swelling, and pain
-
May have fever, chills, or rigor
-
Lactation history including difficulty with breastfeeding, breast engorgement, or chafed nipples [9]
Breast abscess
The following may be seen in those with a breast abscess:
-
Localized breast edema, erythema, warmth, and pain [4]
-
Any history of prior breast infection
-
Lactation history (consider if weaning or returning to work)
-
If not lactating, consider diabetes (polyuria, polydipsia, frequent infections, weight change)
-
Surgical breast intervention within 8 weeks [36]
-
Smoking history
Physical
Perform a thorough breast examination in any patient presenting with a breast complaint and in any older woman presenting with unexplained weight loss, anorexia, or bone pain.
Breast mass
Examine the patient with a breast mass for the following:
-
Firm mass of variable shape and size
-
Observe whether fixed or mobile
-
Fifty percent of masses found in the upper outer quadrant of the breast
-
May have associated pain with palpation (most are painless)
-
Nipple discharge, inversion, changes, or asymmetry
-
Skin retraction or tethering
-
Axillary lymphadenopathy
-
Skin changes - Inflammatory (ie, peau d'orange) or erythematous scaly lesions of the areola (ie, Paget disease) [13]
-
Pay special attention to associated upper-extremity neurologic motor or sensory abnormalities, as these may herald invasion of the brachial plexus—an indication for emergent radiation therapy
Mastitis
Examine the patient with suspected mastitis for the following:
-
Localized breast erythema, warmth, induration, swelling, and tenderness
-
May have associated fever
Breast abscess
Examine the patient with a suspected breast abscess for the following:
-
Localized breast erythema, warmth, induration, edema, and tenderness
-
Most frequently areolar or periareolar (may also be peripheral)
-
Fluctuance, although swelling may limit ability to palpate a mass
-
May have associated fever or axillary lymphadenopathy
-
Nipple discharge or inversion
Causes
Malignant
Risk factors for females include the following:
-
Age older than 40 years
-
Family history of a first-degree relative with breast cancer
-
Menarche before age 12 years
-
Menopause after age 55 years
-
Nulliparity
-
First pregnancy after age 30 years
-
Therapeutic radiation over chest before age 30 years
-
Prediagnosis hormone replacement therapy remains controversial [37]
-
A history of smoking tobacco products for more than 15 years [38]
-
BRCA1 and BRCA2 mutations (responsible for approximately 5% of all breast cancers; inherited in an autosomal dominant fashion; women with mutations in either of these genes have a lifetime risk of breast cancer of 60%-85% and a lifetime risk of ovarian cancer of 15%-40%) [39]
-
Paget disease of the breast [40]
Risk factors for males are as follows [41]
-
BRCA1 and BRCA2 mutations
-
Klinefelter syndrome: 20- to 50-fold greater lifetime risk
-
Cowden syndrome
-
Hormonal imbalance and increased estrogen levels, including liver disease and testicular abnormalities
-
Environmental exposures, including to ionizing radiation, electromagnetic radiation, polycyclic aromatic hydrocarbons, alcohol, and red meat, have been studied in relation to male breast cancer, but none has convincingly been found to be associated with incidence across studies.
Exercise has been shown to decrease the risk of breast cancer in women at high risk for developing a malignancy. However, further studies are needed to verify this association and its relationship to preventing breast cancer in women on tamoxifen therapy (standard treatment for preventing breast cancer recurrence). [38]
Alcohol consumption has not been shown to increase the risk of developing breast cancer. [38]
Benign
Developmental breast lesions
Prepubertal and peripubertal developmental breast lesions may include abnormalities of embryology and gynecomastia.
Abnormalities of embryology include polythelia (accessory nipples) and polymastia (supernumerary breasts).
Gynecomastia is characterized by excessive development of breast tissues in males. It can be physiologic or pathologic in teens.
Neonatal breast hypertrophy is a common transient condition that results from elevation of maternal hormones, seen in up to 90% of all newborns.
Non-developmental breast lesions
Fibrocystic changes
Breast lobules may dilate and form cysts of varying sizes, due to hormonal changes in the menstrual cycle. Cysts are found in about 1 in 3 women aged 35-50 years. [15] Rupturing of the cysts can cause scarring and inflammation that leads to fibrotic changes, which feel rubbery, firm, or hard.
Hyperplasia
Hyperplasia is caused by an overgrowth of cells that line the ducts or lobules. About 1 in 4 women have mild or usual hyperplasia. [15] About 1 in 25 women have atypical hyperplasia (associated with an increased risk of malignancy). [15]
Adenosis
An increase in the number of glands.
Fibroadenoma is the most common cause of breast mass in women younger than 35 years and comprises 91% of all solid breast masses in females younger than 19 years. [42] These arise from the terminal duct lobular unit and appear clinically as singular, firm, rubbery, smooth, mobile, painless masses ranging in size from 1-5 cm. They may grow to a large size, thereby affecting the contours of the overlying skin and overall shape of the breast. Ultrasonography reveals a well-defined hypoechoic homogeneous mass 1-20 cm in diameter. [16, 42] Fibroadenomas appear as multiple masses in 10%-15% of patients. [16]
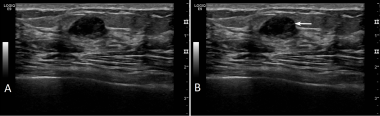 Breast adenoma. A) A breast adenoma is oval with well-defined borders. It may be hypoechoic and some internal echogenicity may be seen. It is wider than tall and posterior acoustic enhancement is NOT seen, helping distinguish from a cyst or other fluid collection. B) An arrow indicates the adenoma.
Breast adenoma. A) A breast adenoma is oval with well-defined borders. It may be hypoechoic and some internal echogenicity may be seen. It is wider than tall and posterior acoustic enhancement is NOT seen, helping distinguish from a cyst or other fluid collection. B) An arrow indicates the adenoma.
 Loculated breast abscess, curvilinear. A) This is the same abscess seen in the above image and is imaged with a curvilinear transducer to better appreciate the extent of the abscess. It is important to image the abscess completely for width and depth. B) The abscess is outlined in yellow and the ribs and posterior acoustic enhancement are noted.
Loculated breast abscess, curvilinear. A) This is the same abscess seen in the above image and is imaged with a curvilinear transducer to better appreciate the extent of the abscess. It is important to image the abscess completely for width and depth. B) The abscess is outlined in yellow and the ribs and posterior acoustic enhancement are noted.
 Purulent breast abscess. A) A purulent breast abscess is seen. The fluid is echogenic, but can be recognized as a disruption of the surrounding tissue and posterior acoustic enhancement. B) The abscess is outlined in yellow and the posterior acoustic enhancement is noted.
Purulent breast abscess. A) A purulent breast abscess is seen. The fluid is echogenic, but can be recognized as a disruption of the surrounding tissue and posterior acoustic enhancement. B) The abscess is outlined in yellow and the posterior acoustic enhancement is noted.
Phyllodes tumor is also known as cystosarcoma phyllodes or giant fibroadenoma. Although generally benign, a malignant variant occurs in 10% of cases. Incidence is highest among women aged 40 to 60 years. Phyllodes tumor is also the most common primary breast malignancy in adolescents. [42] The most common presentation is that of a large (average 5 cm), solitary, firm, breast nodule. Ultrasonographic findings of the mass may appear identical to those of a fibroadenoma with well-circumscribed borders and small cysts. [42]
Papillary adenoma of the nipple [6]
Papillary adenoma is also known as erosive adenomatosis of the nipple, adenoma of the nipple, florid papillomatosis of the nipple, and subareolar duct papillomatosis of the nipple. This is believed to arise from terminal lactiferous ducts. Incidence is highest among women aged 40 to 50 years. It commonly presents with unilateral serous or bloody nipple discharge that increases before menses.
Vascular lesions
Vascular lesions are usually benign. The most common form is hemangioma. Surgical excision may be required. [42]
Infectious
Breast abscess
Puerperal breast abscesses most often contain S aureus and streptococcal species. Methicillin-resistant S aureus (MRSA) has become increasingly common. [26] The overall rate of breastfeeding cessation among patients with breast abscess was 41% in a US cohort and did not differ between MRSA and MSSA infections. [43] In a US cohort, 81% of S aureus–confirmed cultures were MRSA pulsed-field type USA 300–0114. [43] Nonpuerperal abscesses typically contain mixed flora (S aureus, streptococcal species) and anaerobes. [3] Diabetes is strongly associated with incidence and clinical outcomes of breast abscesses in nonlactating women. One study demonstrated a 72% prevalence of diabetes in women with nonpuerperal abscesses. [44] Cigarette smoking is a debated risk factor but has been shown to have a strong association with development of nonpuerperal mastitis. [3, 26, 27, 45, 46] Primary breast abscess has also been reported to be more common in African Americans [27] and those with obesity, [27] and a possible association with inadequate vitamin A supplementation has also been described. [8] Nipple piercing has been associated with increased risk of developing subareolar breast abscess. [46]
 Loculated breast abscess. A) A large loculated abscess is seen containing hypoechoic fluid and some internal echoes. Posterior acoustic enhancement is seen. Care must be taken to image at an adequate depth to visualize posterior borders of breast lesions. B) The abscess is outlined in yellow and the posterior acoustic enhancement is noted.
Loculated breast abscess. A) A large loculated abscess is seen containing hypoechoic fluid and some internal echoes. Posterior acoustic enhancement is seen. Care must be taken to image at an adequate depth to visualize posterior borders of breast lesions. B) The abscess is outlined in yellow and the posterior acoustic enhancement is noted.
Mastitis
Mastitis occurs in up to 33% of lactating women, with its highest incidence within 6 weeks postpartum or while weaning breastfeeding. [18, 47, 48] Periductal mastitis comprises 3%-4% of all benign lesions of the breast. [6] It may be associated with milk stasis caused by ineffective positioning of the baby, limited feeding, or restricted feeding. [9] Of infective mastitis cases, S aureus is the most common cause. Streptococci, enterococci, S epidermidis, Peptostreptococcus species, Prevotella species, and Escherichia coli are less common causes. True fungal mastitis is rare and should prompt evaluation for coexisting diabetes mellitus. In infants, infections with Shigella, E coli, and Klebsiella species have been reported. [22] Mastitis that is refractory to appropriate treatment should prompt evaluation for tuberculous mastitis. [12]
Complications
Potential complications are as follows:
-
Breast mass - Chronic pain, scarring or disfigurement, metastases, postsurgical complications (eg, ipsilateral lymphedema), and death
-
Mastitis - Breast abscess formation in less than 10% of cases
-
Breast abscess - Recurrent infection, scarring, loss of breast size, and noticeable breast asymmetry
-
Chronic breast abscess - Mammary duct fistulization, resection of the nipple-areolar complex [11]
-
Ultrasonogram demonstrates a hypoechoic mass with smooth, partially lobulated margins typical of a fibroadenoma.
-
Craniocaudal mammograms obtained 1 year apart demonstrate a newly developing mass in the outer part of the breast.
-
Spot compression mammogram of the outer part of the breast demonstrates a new mass as smooth, margined, and oval. The findings are consistent with a fibroadenoma, a cyst, or a malignancy. In this patient, the diagnosis was a rapidly growing fibroadenoma.
-
Eggshell or rim calcifications (arrows) have walls thinner than those of lucent-centered calcifications.
-
This mass with associated large, coarse calcifications (arrows) is a degenerating fibroadenoma.
-
Breast cancer, ultrasonography. Mediolateral oblique digital mammogram of the right breast in a 66-year-old woman with a new, opaque, irregular mass approximately 1 cm in diameter. The mass has spiculated margins in the middle third of the right breast at the 10-o'clock position. Image demonstrates both the spiculated mass (black arrow) and separate anterior focal asymmetry (white arrow).
-
Breast cancer, ultrasonography. Antiradial sonogram of the spiculated mass (shown in the image above) demonstrates a hypoechoic mass with angular margins (black arrows). Cursors on the margins of the mass were used to electronically measure its dimensions of the mass, which was 0.9 X 0.8 cm.
-
Breast cyst. A) A simple, fairly round breast cyst with hypo or anechoic contents and well-defined borders; B) Posterior acoustic enhancement is seen as well as edge shadows (arrows).
-
Breast adenoma. A) A breast adenoma is oval with well-defined borders. It may be hypoechoic and some internal echogenicity may be seen. It is wider than tall and posterior acoustic enhancement is NOT seen, helping distinguish from a cyst or other fluid collection. B) An arrow indicates the adenoma.
-
Breast hematoma. A) A breast hematoma is seen as a round echogenic collection with surrounding tissue edema. A hematoma may be hypoechoic, mixed, or fairly echogenic depending on the stage of the hematoma. B) The hematoma is outlined and tissue edema noted.
-
Loculated breast abscess. A) A large loculated abscess is seen containing hypoechoic fluid and some internal echoes. Posterior acoustic enhancement is seen. Care must be taken to image at an adequate depth to visualize posterior borders of breast lesions. B) The abscess is outlined in yellow and the posterior acoustic enhancement is noted.
-
Loculated breast abscess, curvilinear. A) This is the same abscess seen in the above image and is imaged with a curvilinear transducer to better appreciate the extent of the abscess. It is important to image the abscess completely for width and depth. B) The abscess is outlined in yellow and the ribs and posterior acoustic enhancement are noted.
-
Purulent breast abscess. A) A purulent breast abscess is seen. The fluid is echogenic, but can be recognized as a disruption of the surrounding tissue and posterior acoustic enhancement. B) The abscess is outlined in yellow and the posterior acoustic enhancement is noted.
-
Complex breast abscess. In this clip, the features of a loculated breast abscess containing echogenic purulent material are noted. Example of imaging with a linear high-frequency transducer.
-
Loculated breast abscess, curvilinear. In this clip, a large, loculated breast abscess and its features are noted. Example of imaging with a lower-frequency curvilinear transducer to better appreciate the extent of this large abscess.