Laboratory Studies
In patients suspected of having a breast abscess, a CBC count with differential may be helpful. Send an aerobic and anaerobic culture during surgical drainage.
Imaging Studies
Ultrasonography is used to distinguish solid from cystic structures and to direct needle aspiration for abscess drainage. Simple cysts are seen on sonograms as round or oval with sharply defined margins and posterior acoustic enhancement. Complex cysts are characterized by a significant solid component, septations, lobulations, varied wall thickness, and the presence of internal debris. Abscesses usually appear as ill-defined masses with central hypoechoic areas and may display internal septations, debris, posterior enhancement, eccentrically thickened walls, and increased Doppler flow in the walls and surrounding tissue with lack of internal color Doppler flow. [8, 36, 42, 49, 50] The addition of elastography and color Doppler ultrasonography to B-mode ultrasonography has been reported to increase the positive predictive value (PPV) of screening ultrasonography in women with dense breasts (from 8.9% to 23.2%; P< .001]) while reducing the number of false-positive findings without missing cancers. [51, 52] Thus, ultrasonography may be particularly useful in younger patients (< 40 years). [53] In addition, ultrasound-guided biopsy has been shown to be safe and effective. [54]
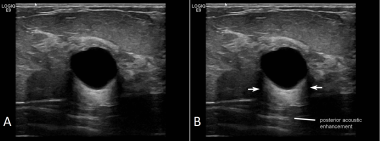 Breast cyst. A) A simple, fairly round breast cyst with hypo or anechoic contents and well-defined borders; B) Posterior acoustic enhancement is seen as well as edge shadows (arrows).
Breast cyst. A) A simple, fairly round breast cyst with hypo or anechoic contents and well-defined borders; B) Posterior acoustic enhancement is seen as well as edge shadows (arrows).
Contrast-enhanced ultrasonography has also been found to be helpful in distinguishing benign from malignant breast masses. This modality has been shown to be 86% sensitive and 79% specific for differentiating between the two types of masses. [55] For more information, see Breast Cancer, Ultrasonography.
It should be noted that although bedside ultrasound performed in the emergency department (ED) by trained emergency medicine providers (rather than by radiology) may effectively identify an abscess, [56] patient selection is important. In one study, 40% of ED bedside studies were incomplete/inadequate, and 21% of cancers were not identified. [57]
Various types of breast masses are shown in the images below.
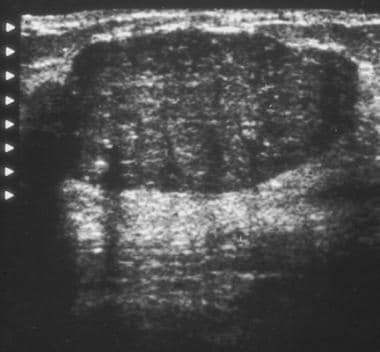 Ultrasonogram demonstrates a hypoechoic mass with smooth, partially lobulated margins typical of a fibroadenoma.
Ultrasonogram demonstrates a hypoechoic mass with smooth, partially lobulated margins typical of a fibroadenoma.
 Breast cancer, ultrasonography. Mediolateral oblique digital mammogram of the right breast in a 66-year-old woman with a new, opaque, irregular mass approximately 1 cm in diameter. The mass has spiculated margins in the middle third of the right breast at the 10-o'clock position. Image demonstrates both the spiculated mass (black arrow) and separate anterior focal asymmetry (white arrow).
Breast cancer, ultrasonography. Mediolateral oblique digital mammogram of the right breast in a 66-year-old woman with a new, opaque, irregular mass approximately 1 cm in diameter. The mass has spiculated margins in the middle third of the right breast at the 10-o'clock position. Image demonstrates both the spiculated mass (black arrow) and separate anterior focal asymmetry (white arrow).
 Breast cancer, ultrasonography. Antiradial sonogram of the spiculated mass (shown in the image above) demonstrates a hypoechoic mass with angular margins (black arrows). Cursors on the margins of the mass were used to electronically measure its dimensions of the mass, which was 0.9 X 0.8 cm.
Breast cancer, ultrasonography. Antiradial sonogram of the spiculated mass (shown in the image above) demonstrates a hypoechoic mass with angular margins (black arrows). Cursors on the margins of the mass were used to electronically measure its dimensions of the mass, which was 0.9 X 0.8 cm.
Schedule an outpatient mammography to further characterize the suspected breast mass. The sensitivity of mammography ranges from 74%-95%, and specificity ranges from 89%-99%. [58, 59] In a meta-analysis of more than 8.5 million patients, the AUC of mammography for breast cancer screening was 0.95, the overall sensitivity was 0.81, and the overall specificity was 0.96. [60] A subgroup analysis of dense-breast populations showed that the combined sensitivity and specificity of mammography was 0.74 and 0.93, respectively. [60]
Early detection with screening mammography significantly reduces breast cancer–related mortality by 20% to 40%. [61] Annual screening mammography of women aged 40-84 years prevents more deaths due to breast cancer than biennial screening of women aged 50 to 74 years. [61] Currently, supplemental screening with ultrasonography or MRI is recommended in addition to mammography. [61] The American Cancer Society recommends annual screening mammography and supplemental screening MRI in women with an estimated lifetime risk of breast cancer of 20%, BRCA mutation carriers, first-degree relatives of BRCA mutation carriers who remain untested, women with a history of mediastinal irradiation aged 10-30 years, and women with certain genetic syndromes. [61] With aggressive public screening, the incidence of large breast tumors may be decreasing. [62] However, with increased screening comes the risk of overdiagnosis.
Approximately 5%-10% of screening examinations are interpreted as abnormal, but 90% of women with abnormal results do not have breast cancer. [58, 59] For instance, the Canadian National Breast Screening Study concluded that approximately 30% of invasive screen-detected breast cancers in women aged 40 to 49 years and 20% of those screen-detected in women aged 50 to 59 years were overdiagnosed. [63] Moreover, a subsequent meta-analysis reported no significant effect on either breast cancer mortality or all-cause mortality when breast cancer screening was extended to women aged 40 to 49 years, but the rates of overdiagnosis were estimated to be 32% at 5 years following cessation of screening and 48% at 20 years following cessation. [64] For these reasons (and others), current guidelines do not recommend extending routine mammography screening to younger age groups. [64] However, when screening women with dense breasts, the addition of bedside ultrasonography may be useful. In a cohort of 66,680 women undergoing physician-performed ultrasonography in addition to mammography, the sensitivity of mammography with ultrasonography rose from 61.5% to 81.3%. [65]
Racial disparities in utilization of screening mammography are evident in black and Hispanic populations in the United States. [66] Further studies are needed to understand reasons for disparities, trends over time, and the effectiveness of interventions targeting these disparities. [66]
For more information, see Breast, Benign Calcifications, Breast, Fibroadenoma, Breast, Nipple Discharge Evaluation, and Breast Cancer, Mammography.
Supplemental ultrasonography improves cancer detection in screening of women at average risk. When comparing screening with mammography alone versus mammography plus physician–performed ultrasonography in average-risk women, the overall sensitivity of mammography alone was 86.6% (non-dense breast) and 61.5% (dense breast) versus 95% (non-dense breast) and 81.3% (dense breast) for mammography with ultrasonography. [65] Adjunctive ultrasonography increased the recall rate from 10.5 to 16.5 per 1000 women screened and increased the biopsy rate from 6.3 to 9.3 per 1000 women screened. [65] The positive predictive value of biopsy was 55.5% for mammography alone and 43.3 for combined mammography plus ultrasonography. [65]
Computer-aided digital breast tomosynthesis is a new imaging modality that has shown some promise as an additional (or even sole) screening tool for breast cancer. Current studies of computer-aided digital breast tomosynthesis show sensitivity of detecting masses and microcalcifications ranging between 85% and 89%. Its utility in detecting masses in dense breast tissue is still a debated topic. Current US guidelines have recommended against its routine use. [67]
MRI may also be helpful in select cases. On diffusion-weighted imaging (DWI), profoundly low apparent diffusion coefficient values were a distinguishing sign of breast abscess due to necrotic breast cancer. [68]
Various breast masses are shown in the mammograms below.
 Craniocaudal mammograms obtained 1 year apart demonstrate a newly developing mass in the outer part of the breast.
Craniocaudal mammograms obtained 1 year apart demonstrate a newly developing mass in the outer part of the breast.
 Spot compression mammogram of the outer part of the breast demonstrates a new mass as smooth, margined, and oval. The findings are consistent with a fibroadenoma, a cyst, or a malignancy. In this patient, the diagnosis was a rapidly growing fibroadenoma.
Spot compression mammogram of the outer part of the breast demonstrates a new mass as smooth, margined, and oval. The findings are consistent with a fibroadenoma, a cyst, or a malignancy. In this patient, the diagnosis was a rapidly growing fibroadenoma.
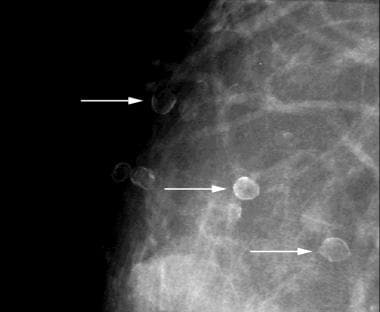 Eggshell or rim calcifications (arrows) have walls thinner than those of lucent-centered calcifications.
Eggshell or rim calcifications (arrows) have walls thinner than those of lucent-centered calcifications.
Procedures
Breast abscesses may be drained with incision and drainage (versus ultrasound-guided needle aspiration and irrigation). Historically, incision and drainage was considered the standard of care for abscesses. Although this method has a lower reoccurrence rate, it is more invasive than needle aspiration and frequently results in scarring with structural damage and poor cosmetic outcomes. [69] Fine-needle aspiration should be considered first-line therapy for abscesses smaller than 5 cm owing to its lower risks, followed by incision and drainage if recurrence occurs. [4] Surgical excision may be required for infected or obstructed lactiferous ducts and provides a lower rate of recurrence for nonpuerperal abscess and mastitis. [70, 8]
Ultrasound-guided needle aspirations are more successful on abscesses smaller than 3 cm and on puerperal abscesses. [71, 72, 73, 8] Loculations are associated with failure of resolution with aspiration, regardless of abscess volume. [74] Nonpuerperal abscesses have a higher rate of recurrence and often require multiple drainage attempts. [8] Regardless of the underlying organism, the need for repeat aspiration is common in patients treated with aspiration versus incision and drainage. [75] In a US cohort of 54 abscess cases treated with needle-guided aspiration, the median number of drainage procedures was 2 (interquartile range, 1.0-4.0), with 24% requiring 5 or more drainage procedures. [43]
Vacuum-assisted biopsy is a viable option for the management of lactational breast abscesses and has been associated with a shorter healing time than simple needle aspiration. [76] Furthermore, percutaneous catheter drainage may be considered for larger abscesses. [4, 77]
Ultrasonographic elastography with virtual touch tissue quantification (VTQ) is used to characterize breast lesions and to analyze the stiffness of glandular and subcutaneous fatty tissue in benign and malignant lesions. [78, 79] Acoustic radiation force impulse imaging is used to measure shear wave velocity (SWV), which reflects the stiffness of tissue. Tissue stiffness is measured within the lesion (internal SWV-SWVi) , in the boundary zone (SWVb), in normal‐appearing glandular tissue (SWVg), and in subcutaneous fatty tissue (SWVf). SWVs inside and at the edge of a breast mass are important for determining if they are benign or malignant. All types of SWVs were significantly higher in the malignant group than the benign group (P< 0.05).
-
Ultrasonogram demonstrates a hypoechoic mass with smooth, partially lobulated margins typical of a fibroadenoma.
-
Craniocaudal mammograms obtained 1 year apart demonstrate a newly developing mass in the outer part of the breast.
-
Spot compression mammogram of the outer part of the breast demonstrates a new mass as smooth, margined, and oval. The findings are consistent with a fibroadenoma, a cyst, or a malignancy. In this patient, the diagnosis was a rapidly growing fibroadenoma.
-
Eggshell or rim calcifications (arrows) have walls thinner than those of lucent-centered calcifications.
-
This mass with associated large, coarse calcifications (arrows) is a degenerating fibroadenoma.
-
Breast cancer, ultrasonography. Mediolateral oblique digital mammogram of the right breast in a 66-year-old woman with a new, opaque, irregular mass approximately 1 cm in diameter. The mass has spiculated margins in the middle third of the right breast at the 10-o'clock position. Image demonstrates both the spiculated mass (black arrow) and separate anterior focal asymmetry (white arrow).
-
Breast cancer, ultrasonography. Antiradial sonogram of the spiculated mass (shown in the image above) demonstrates a hypoechoic mass with angular margins (black arrows). Cursors on the margins of the mass were used to electronically measure its dimensions of the mass, which was 0.9 X 0.8 cm.
-
Breast cyst. A) A simple, fairly round breast cyst with hypo or anechoic contents and well-defined borders; B) Posterior acoustic enhancement is seen as well as edge shadows (arrows).
-
Breast adenoma. A) A breast adenoma is oval with well-defined borders. It may be hypoechoic and some internal echogenicity may be seen. It is wider than tall and posterior acoustic enhancement is NOT seen, helping distinguish from a cyst or other fluid collection. B) An arrow indicates the adenoma.
-
Breast hematoma. A) A breast hematoma is seen as a round echogenic collection with surrounding tissue edema. A hematoma may be hypoechoic, mixed, or fairly echogenic depending on the stage of the hematoma. B) The hematoma is outlined and tissue edema noted.
-
Loculated breast abscess. A) A large loculated abscess is seen containing hypoechoic fluid and some internal echoes. Posterior acoustic enhancement is seen. Care must be taken to image at an adequate depth to visualize posterior borders of breast lesions. B) The abscess is outlined in yellow and the posterior acoustic enhancement is noted.
-
Loculated breast abscess, curvilinear. A) This is the same abscess seen in the above image and is imaged with a curvilinear transducer to better appreciate the extent of the abscess. It is important to image the abscess completely for width and depth. B) The abscess is outlined in yellow and the ribs and posterior acoustic enhancement are noted.
-
Purulent breast abscess. A) A purulent breast abscess is seen. The fluid is echogenic, but can be recognized as a disruption of the surrounding tissue and posterior acoustic enhancement. B) The abscess is outlined in yellow and the posterior acoustic enhancement is noted.
-
Complex breast abscess. In this clip, the features of a loculated breast abscess containing echogenic purulent material are noted. Example of imaging with a linear high-frequency transducer.
-
Loculated breast abscess, curvilinear. In this clip, a large, loculated breast abscess and its features are noted. Example of imaging with a lower-frequency curvilinear transducer to better appreciate the extent of this large abscess.